Commissioner of Customs and Excise reviews Hong Kong Customs passing-out parade (with photos)
The Commissioner of Customs and Excise, Ms Louise Ho, attended the Passing-out Parade for the 140th-143rd Inspector Induction Courses and the 496th-501st Customs Officer Induction Courses at the Hong Kong Customs College today (December 17) to inspect 70 Probationary Inspectors and 115 Probationary Customs Officers on parade.
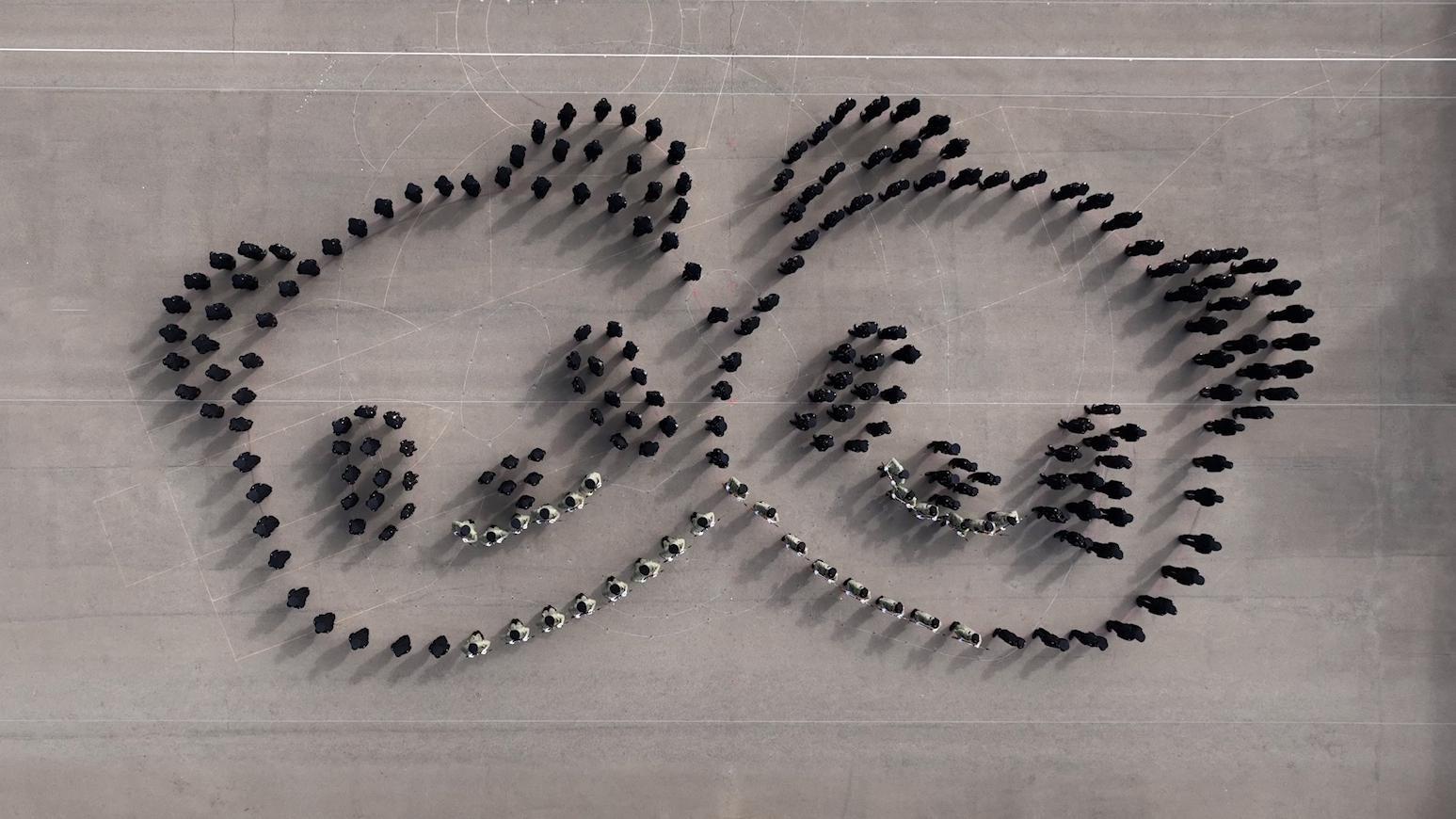
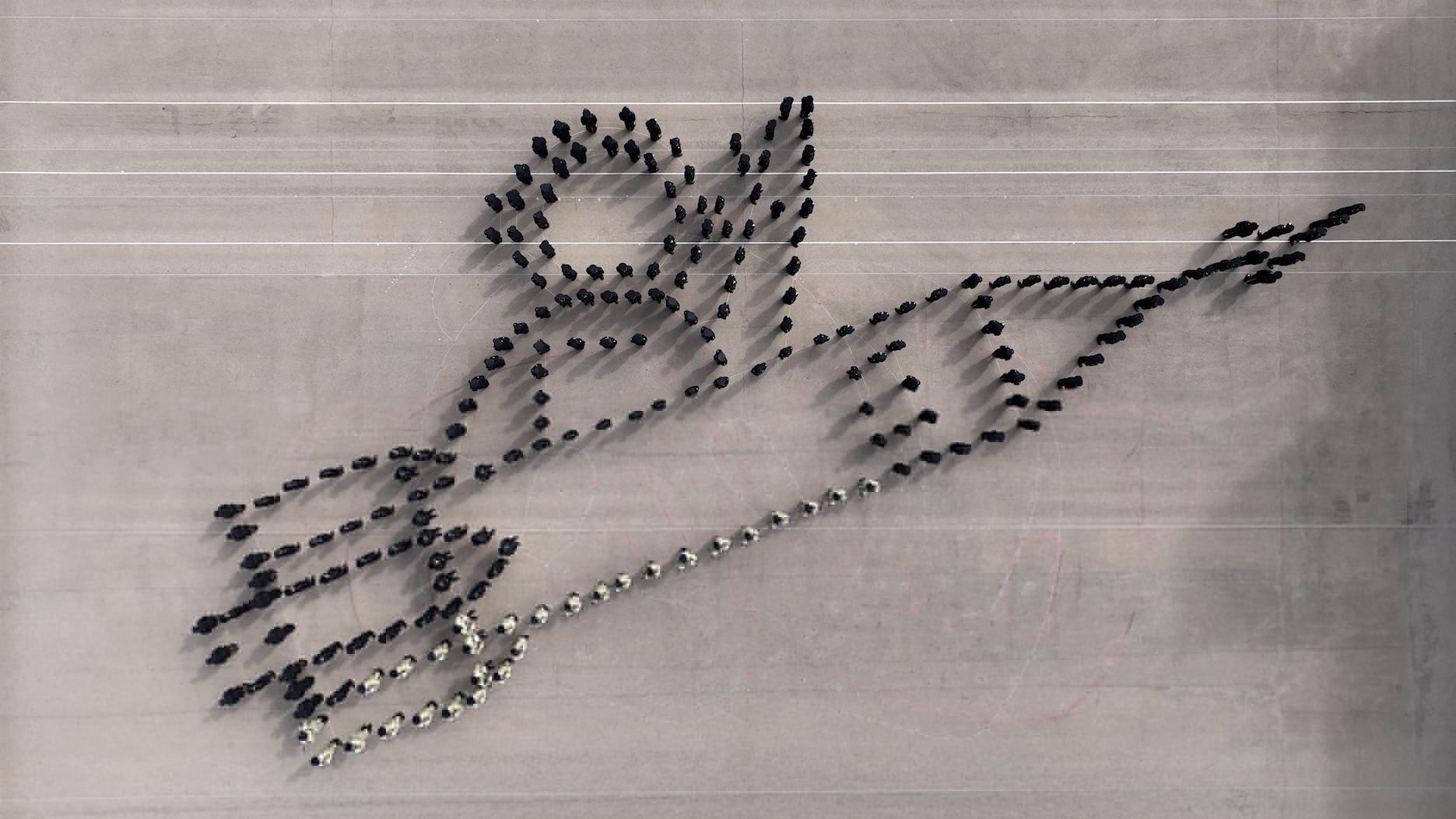
The Guards of Honour and all passing-out officers adopted the Chinese-style foot drill to form one big and two small patterns of giant pandas, representing the giant pandas gifted by the Central Government and the first giant panda twins born in Hong Kong. Next, they formed the pattern of a rocket and an astronaut in celebration of the successful launch of the Shenzhou-19 manned spaceflight mission. This arrangement demonstrated Hong Kong Customs’ patriotic feeling and affection for the country and Hong Kong.
Speaking at the passing-out parade, Ms Ho said Customs is committed to leveraging Hong Kong’s distinctive advantages of enjoying strong support of the motherland while being closely connected to the world under “one country, two systems”. The department actively enhances international and regional collaborations by developing Belt and Road partnerships in the Association of Southeast Asian Nations, the Middle East, Central Asia and Africa to consolidate Hong Kong’s international status and give full play to its role as the bridge between the Mainland and the rest of the world.
She added that Customs dares to play a more significant role in the international arena. With the support of the Central Government and the Hong Kong Special Administrative Region Government, Hong Kong Customs represented Hong Kong, China to assume the position of the Vice-Chairperson for the Asia/Pacific region of the World Customs Organization in July this year for a term of two years, shouldering the responsibilities of driving and co-ordinating regional development and affairs, leading members to cope with challenges, formulating strategies to address issues of common concern and charting the way forward. Hong Kong Customs spares no effort in fulfilling the leadership role and strengthening Hong Kong’s roles as the “super-connector” and the bridgehead to to enhance the country’s and Hong Kong’s international voice and influence.
Ms Ho encouraged the passing-out officers to fully achieve Hong Kong Customs’ goal of creating “a new chapter of Asia-Pacific customs collaboration” by providing quality and diversified Customs services to make contributions to the country and Hong Kong.